If a cell suffers damage to its DNA while in S phase, how can this damage be repaired before the cell enters mitosis?
How do translocations such as the Philadelphia chromosome contribute to cancer?
 Verified step by step guidance
Verified step by step guidance
Verified video answer for a similar problem:
Key Concepts
Chromosomal Translocations

Philadelphia Chromosome

Oncogene Activation and Cancer Development
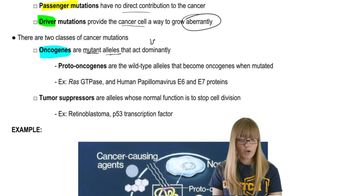
Distinguish between oncogenes and proto-oncogenes. In what ways can proto-oncogenes be converted to oncogenes?
Of the two classes of genes associated with cancer, tumor-suppressor genes and oncogenes, mutations in which group can be considered gain-of-function mutations? In which group are the loss-of-function mutations? Explain.
How do normal cells protect themselves from accumulating mutations in genes that could lead to cancer? How do cancer cells differ from normal cells in these processes?
Radiotherapy (treatment with ionizing radiation) is one of the most effective current cancer treatments. It works by damaging DNA and other cellular components. In which ways could radiotherapy control or cure cancer, and why does radiotherapy often have significant side effects?
Genetic tests that detect mutations in the BRCA1 and BRCA2 tumor-suppressor genes are widely available. These tests reveal a number of mutations in these genes—mutations that have been linked to familial breast cancer. Assume that a young woman in a suspected breast cancer family takes the BRCA1 and BRCA2 genetic tests and receives negative results. That is, she does not test positive for the mutant alleles of BRCA1 or BRCA2. Can she consider herself free of risk for breast cancer?
