Developing SEMH provision by focusing on pupil wellbeing

SENDCO Kat Dockery on interpreting and implementing the CASCADE framework in order to improve children's and young people's mental health and wellbeing.
In September 2014, the Government established the Children and Young People’s Mental Health Taskforce[1], aiming to identify what needs to be done to improve children and young people’s mental health and wellbeing.
There was a clear focus on making it easier to access help and support and improving how children and young people’s mental health services are organised, commissioned and provided.
The Taskforce outlined a number of proposals to help improve access to effective support for children and young people. The proposals, which were published in the report, Future in Mind[2] included the establishment of a named point of contact within CAMHS (Child and Adolescent Mental Health Services) and a named lead within each school.
The named lead is responsible for mental health and developing closer relationships with NHS CAMHS in support of timely and appropriate referrals to specialist services and recommending the development of a joint training programme.
Exploring the pilot
The Children and Young People’s Mental Health Taskforce pilot aimed to examine how training and subsequent joint working can improve local knowledge and identification of mental health issues, as well as improving referrals to specialist services. The hope was to successfully establish (and reset) the boundaries of what schools can do, where schools and NHS CAMHS can work together, and where schools needs to hand over for more specialist support.
As the named lead for my school, I was able to fully participate in the training and development of the joint working models drawing on the overview of mental health knowledge that I possessed within the school.
Sean Jordan was our Youth and Wellbeing worker. We initially met together with all of the participants of the pilot in our area to discuss CAMHS and our schools’ current concerns. During this session, we were introduced to the CASCADE framework[3].
The CASCADE framework
The Anna Freud Centre, who had responsibility for delivering all the training sessions and hosted two national events to share learning and best practice, provided the CASCADE model within the first training session showcasing it as an audit tool for everyone to baseline their current practise.
| Major challenge | Good elements of practice | Widespread good practice | Gold Standard | |
|---|---|---|---|---|
| Clarity on roles, remit, and responsibilities of all partners involved in supporting CYP mental health | No shared knowledge of the range of support available and poor links between partners | Some shared knowledge of the range of support available. Some links between partners | Shared knowledge of support available and good links between partners | Full mapping of all sources of support key up-to-date and accessible with strong links between all partners |
| Agreed point of contact and role in schools and CYP mental health services | No identified points of contact | Some identified points of contact with partners | Agreed and shared points of contact with most partners | Agreed and shared points of contact with all partners that are kept up to date as staff change |
| Structures to support shared planning and collaborative working | No structures to support shared planning and collaborative working | Steering group or partnership agreement or other structure to support shared planning and collaborative working but membership attendance patchy or frequently cancelled | Steering group or partnership agreement or other structure to support shared planning and collaborative working but not fully linked to other groups | Steering group or partnership agreement or other structure to support shared planning and collaborative working, embedded well with other relevant groups |
| Common approach to outcome measures for young people | No shared outcome measures and no sharing of information | Some overlap of outcome measures, but no shared information | Most shared outcome measures and limited sharing of outcomes | Routine use of shared outcome measures that are routinely shared |
| Ability to continue to learn and draw on best practice | No forum for shared learning | Some sharing at joint events with some partners or access to good practice networks but limited | Widespread sharing of best practice with most partners but not always acted upon | Widespread sharing of evidence based best practice with all partners that drives initiatives |
| Development of integrated working to promote rapid and better access to support | Little to no integrated working and complicated and/or slow path(s) to support | Some integrated working with partners to improve access despite complicated and/or slow paths to support | Widespread integrated working with most partners to improve access with clear path to support | Widespread integrated working with all partners to improve access with clear and/or rapid path to support |
| Evidence based approach to intervention | Little or limited training available to support intervention, and not grounded in evidence. | Some routine training available, but not always evidence-based. Some interventions in place | Most staff accessing regular targeted training with interventions in place | Clear training programme for all staff with some joint training alongside interventions |
This framework gave us a strategic overview of what to aim for when developing our SEMH provision in collaboration with mental health services. The CASACDE model sets out a list of standards and a set of criteria for each one, ranging from ‘major challenge’ to ‘gold standard’. This allowed us to pinpoint our current position and set targets in order to improve our SEMH provision and the support our pupils receive, whether it is inside or outside of school.
Our interpretation of the framework
After meeting with our mental health link worker, we set up a plan for our school’s needs learning how to assess mental health and how to target support. Our overall aim was to generate the skills we needed to become self-sufficient in delivering high quality, highly effective SEMH provision for our pupils.
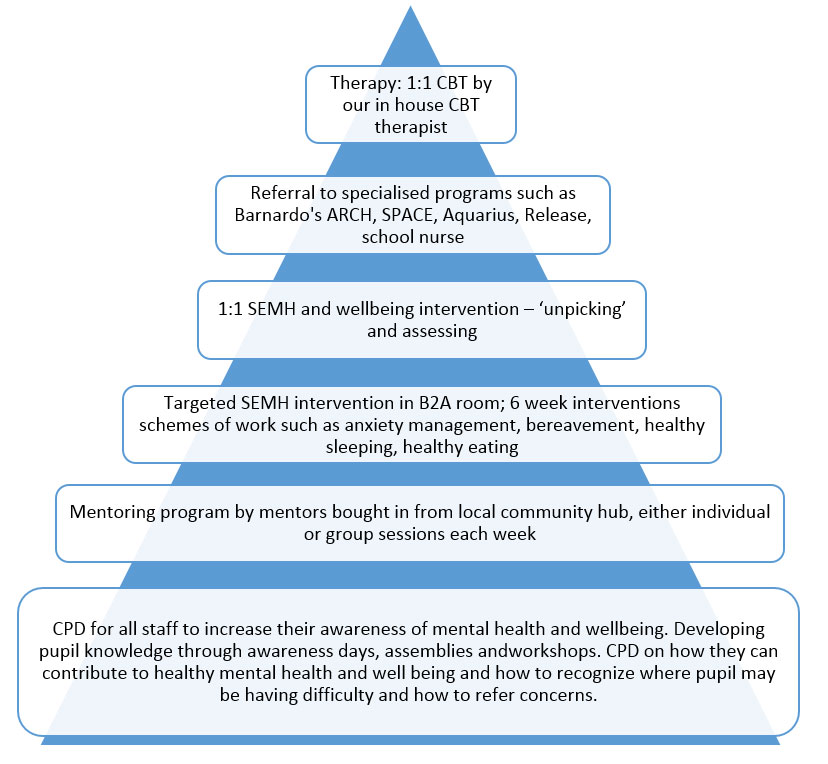
Our learnings led us to creating our own tiered model of support.
Step one
The first step of our model is to ensure all staff have an awareness of mental health, which we deliver through CPD. It is most important to bring the mental health into the context of learning; changing the understanding that mental health will impact on the ability to learn.
Step two
The next step is ensuring that the young people themselves have an awareness of mental health, which we complete through mental health awareness days, assemblies and workshops.
We found that through these initial steps alone, the referral numbers from staff and self-referrals from pupils became extremely high.
Increasing awareness brought many pupils to us who previously may have been left to suffer for longer, having a detrimental effect on their long-term mental health.
By raising awareness, we were able to signpost help and intervene early to prevent escalation.
Step two is mentoring; we have a contract with our local community hub who work with many of our pupils outside of school hours in the community and on youth projects. Our mentors run individual or group sessions connected with pupil attitude and social behaviour. These can be personalised project such as boxing, exploring role models or family activities.
Step three
Step three is targeted intervention. These referrals come through from pastoral teams, SENDCO or self-referral by pupils for specific issues such as issues with diet, sleep, self-esteem, bereavement, anxiety, friendships, anger management and family difficulties.
We have specific schemes of work, which the pupils work through for an hour a week, over a six to eight week period, with a member of staff. As a result, pupils feel that they have committed time to working through their issues and feel they gain strategies of how to cope better with, or how to resolve, their difficulty.
Step four
Step four is used when pupils are referred but their issues are unclear. Perhaps a teacher has noticed a pupil’s wellbeing has deteriorated but we are unaware as to why, for example.
Here our Youth and Wellbeing team will meet 1:1 with pupils for several sessions to get to know them, build up a relationship and work on encouraging positive experiences (such as baking a cake together if the pupil likes to cook).
The pupils usually then open up during this period of time and strategies are put in place with their worker in order to help pupils resolve their difficulties and improve their wellbeing.
At this stage we also use mental health assessments such as the R-CAD (Revised Childrens Anxiety and Depression Scale) so that we can assess their mental health upon entry to the 1:1 sessions.
Here we can identity what the specific mental health issue may be from social phobia, panic disorder, depression, separation anxiety, generalised anxiety and obsessive–compulsive and also the degree of severity of the disorder. Use of this assessment tool gives the wellbeing workers a sense of the pupils starting point and specifically what they need to work on.
The R-CADs are then completed again six to eight weeks later to see the level of improvement made by the pupils and the impact the sessions have had.
Step five
Step five is used when the Wellbeing workers feel a more specialist approach is required for a specific concern. For example if a pupils wellbeing is affected due to drug use we will refer out to Aquarius or if emotional resilience is a concern we refer to Barnardo’s ARCH project.
At this point, if we are unsure, we can call Forward Thinking Birmingham to be signposted as to where to gain support.
Step six
Step six is referral for Cognitive Behaviour Therapy sessions one or twice a week with our B2A manager who is a qualified Cognitive Behaviour Therapist. Pupils will access this support for six to eight weeks and may also follow up with stage three support if a particular issue is discovered during CBT sessions.
Ultimately, by taking part in this pilot, we have developed a better understanding of our capacity and capability to support our pupils with mental health needs.
We have a stronger working relationship with NHS CAMHS, ensuring the correct support is signposted early on and effective support follows. We believe that other schools can achieve the same outcomes.
Download 'Future in Mind' from the UK Government website for further information
Sign-up to receive Education and SEND enews for more blog posts like this
by Kat Dockery
About the author
Kat Dockery is a SENDCo in a mainstream secondary Academy in Birmingham. Formerly a science teacher, Kat became Head of a Specialist ASC Resource Base within her setting before taking the role of SENDCo.
She has been deployed as a Specialist Leader in Education for Academies Enterprise Trust and the London Leadership Strategy supporting School-to-School SEND Reviews. Kat has worked with schools locally providing peer to peer support for provision development.