Calculate the decimal reduction time (D) for the two temperatures in the following graph.
Ch. 9 - Controlling Microbial Growth in the Environment

Bauman6th EditionMicrobiology with Diseases by TaxonomyISBN: 9780134832302Not the one you use?Change textbook
Chapter 9, Problem 1
Describe three types of microbes that are extremely resistant to antimicrobial treatment, and explain why they are resistant.
 Verified step by step guidance
Verified step by step guidance1
Identify three types of microbes known for their extreme resistance to antimicrobial treatments. Common examples include bacterial endospores, mycobacteria, and certain protozoan cysts.
Explain bacterial endospores: These are dormant, tough structures formed by some bacteria (e.g., Bacillus and Clostridium species). Their resistance comes from a thick protective coat, low water content, and metabolic inactivity, which protect them from heat, chemicals, and radiation.
Describe mycobacteria: These bacteria (e.g., Mycobacterium tuberculosis) have a unique cell wall rich in mycolic acids, which makes them impermeable to many antibiotics and disinfectants, contributing to their resistance.
Discuss protozoan cysts: Some protozoa form cysts with a thick, protective outer layer that shields them from harsh environmental conditions and antimicrobial agents, allowing them to survive until conditions improve.
Summarize that the resistance mechanisms involve structural barriers, metabolic states, and protective layers that prevent antimicrobial agents from reaching or effectively acting on these microbes.

Verified video answer for a similar problem:
This video solution was recommended by our tutors as helpful for the problem above.
Video duration:
51sWas this helpful?
Key Concepts
Here are the essential concepts you must grasp in order to answer the question correctly.
Types of Microbes Resistant to Antimicrobial Treatment
Certain microbes such as bacterial spores, mycobacteria, and biofilm-forming bacteria exhibit high resistance to antimicrobials. Bacterial spores are dormant forms that survive harsh conditions. Mycobacteria have a waxy cell wall that limits drug penetration. Biofilms are communities of microbes encased in a protective matrix that impedes antimicrobial access.
Recommended video:
Guided course
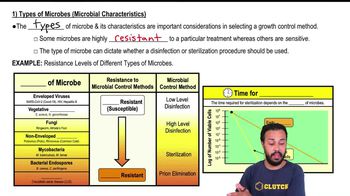
Types of Microbes (Microbial Characteristics)
Mechanisms of Microbial Resistance
Microbes resist antimicrobials through various mechanisms including reduced permeability, enzymatic drug degradation, efflux pumps, and altered target sites. For example, mycobacteria’s mycolic acid layer reduces drug entry, while biofilms physically block drugs. Understanding these mechanisms explains why some microbes survive treatments that kill others.
Recommended video:
Guided course

Introduction to Avoiding Host Defense Mechanisms
Clinical Implications of Antimicrobial Resistance
Resistance in microbes complicates infection treatment, leading to persistent infections and increased healthcare costs. Resistant microbes require higher drug doses or alternative therapies, which may have more side effects. Recognizing resistant microbes helps guide effective treatment strategies and infection control measures.
Recommended video:
Guided course
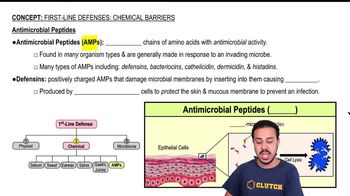
Antimicrobial Peptides
Related Practice
Textbook Question
703
views
Textbook Question
In practical terms in everyday use, which of the following statements provides the definition of sterilization?
a. Sterilization eliminates all organisms and viruses
b. Sterilization eliminates harmful microorganisms and viruses
c. Sterilization eliminates prions
d. Sterilization eliminates hyperthermophiles
513
views
Textbook Question
Which of the following substances or processes kills microorganisms on laboratory surfaces?
a. Antiseptics
b. Disinfectants
c. Degermers
d. Pasteurization
572
views
Textbook Question
Compare and contrast four tests that have been developed to measure the effectiveness of disinfectants.
540
views
Textbook Question
Which of the following terms best describes the disinfecting of cafeteria plates?
a. Pasteurization
b. Antisepsis
c. Sterilization
d. Sanitization
529
views
